Medicare Reimbursement Calculator: Complete Guide
In 2025, Medicare reimbursement calculators have become essential for billing teams aiming to estimate payouts accurately, reduce denials, and stay compliant. These tools calculate expected payments based on CPT/HCPCS codes, modifiers, and location-specific factors, helping avoid underbilling and revenue loss.
As CMS rules grow stricter, even minor mistakes can trigger audits. Calculators now factor in RVUs, GPCI, and conversion rates for precise pre-claim validation. Teams familiar with reimbursement workflows use these tools not just for estimates—but for better financial forecasting, cleaner submissions, and faster payments.
What Is a Medicare Reimbursement Calculator?
A Medicare reimbursement calculator is a web- or software-based tool that estimates the amount Medicare will reimburse for specific medical services or procedures. It accounts for critical variables like CPT or HCPCS codes, place of service (POS), applicable modifiers, provider type, and geographic locality. By aligning with CMS’s fee schedule methodology, the tool offers a real-time estimate of what Medicare is likely to pay for a claim—before it's submitted.
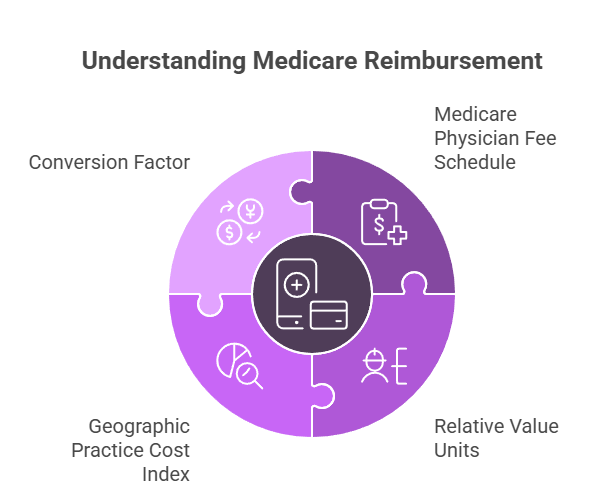
These calculators are powered by the Medicare Physician Fee Schedule (MPFS) and apply additional adjustments based on Relative Value Units (RVUs), the Geographic Practice Cost Index (GPCI), and the conversion factor. Some also include built-in warnings for codes that are non-billable, bundled, or missing essential modifiers—minimizing coding errors before they reach payers.
In outpatient billing, calculators assist with services where payment varies based on setting (e.g., office vs. ASC), or when technical and professional components are billed separately. In inpatient environments, they can estimate allowable rates for procedures falling under global billing packages or DRG-based systems. For suppliers and DME providers, calculators help determine reimbursement rates for durable medical equipment (DME) such as oxygen tanks or wheelchairs—based on item type, purchase/rental status, and region. More on this is covered in the DME coding guide.
Used proactively, these calculators help billing teams anticipate Medicare’s allowed amount, the limiting charge, and even potential patient responsibility. They’re especially useful during pre-authorization, charge review, and denial management—serving as a safeguard against costly claim resubmissions and audit exposure.
Quick Snapshot: What Medicare Reimbursement Calculators Do
- Estimate payouts using CPT/HCPCS codes, POS, modifiers, and locality
- Reference MPFS, RVUs, GPCI, and the conversion factor for accuracy
- Flag non-billable or bundled codes before submission
- Handle outpatient, inpatient, and DME billing scenarios
- Support pre-auth, charge review, and denial prevention workflows
Key Components That Affect Medicare Reimbursement
To interpret calculator results accurately, billers must understand the elements that shape Medicare’s reimbursement formulas. Each component plays a unique role in determining what Medicare will pay.
1. Medicare Physician Fee Schedule (MPFS)
This schedule is the foundation of all fee-for-service Medicare billing. It lists national base payment rates for covered CPT and HCPCS codes. Each service has associated values that reflect the resources required, including clinician time, practice costs, and patient risk.
2. Relative Value Units (RVUs)
Every code carries three RVUs:
Work RVU – effort, skill, and time required by the provider
Practice Expense RVU – cost of maintaining the practice environment
Malpractice RVU – the professional liability expense component
These values are multiplied and adjusted based on geography to derive the total payment amount.
3. Geographic Practice Cost Index (GPCI)
Medicare adjusts RVUs using the GPCI to reflect regional cost differences. For instance, a code billed in San Francisco may be reimbursed at a higher rate than the same code billed in rural Ohio due to overhead cost differences.
4. Conversion Factor
This is a dollar multiplier Medicare applies to the GPCI-adjusted RVUs to calculate final payment. The conversion factor changes yearly, often influenced by federal budget negotiations and CMS policy updates.
Correct CPT code selection is crucial for calculator accuracy. A mismatched code, missing modifier, or failure to update old codes will result in flawed estimations—often leading to denials, resubmissions, or underpayments that impact revenue cycle health.
How to Use a Reimbursement Calculator Step-by-Step
Using a Medicare reimbursement calculator correctly requires attention to detail. A small oversight—like the wrong modifier or place of service—can result in skewed estimates and claim errors. Here’s a step-by-step guide to getting accurate results.
1. Select Your CPT or HCPCS Code
Begin by entering the CPT or HCPCS code for the procedure or service. Be sure the code is current and matches the documented service precisely. For DME, ensure you’re using the proper HCPCS Level II code and item description.
2. Enter the Place of Service (POS)
Select the correct POS code—for example, 11 for an office, 22 for outpatient hospital, or 31 for skilled nursing. Medicare rates differ significantly depending on where care is rendered.
3. Add Applicable Modifiers
Include any modifiers that apply to the service (e.g., -26 for professional component, -TC for technical, or -59 for distinct services). Incorrect modifier use can inflate or reduce reimbursement inappropriately.
4. Choose Locality or ZIP Code
Medicare uses the Geographic Practice Cost Index (GPCI) to adjust payments by region. Enter the ZIP code or select from the provided carrier locality dropdowns. This will ensure your RVUs are GPCI-adjusted.
5. Interpret the Results
The calculator will output key values:
Medicare allowable amount (what Medicare pays before deductible/copay)
Limiting charge (for non-participating providers)
Patient responsibility under Medicare rules
If you see errors, check for mismatched codes, invalid modifiers, or outdated CPTs. It’s also important to check whether global surgical periods affect payment timing or bundling.
Example Calculation
Let’s say you enter CPT 99214 (office visit), POS 11, no modifiers, ZIP code 10001 (New York). The calculator might return:
Allowable: $121.80
Limiting charge: $139.07 (if non-par)
Medicare pays: 80% of allowable after deductible
Using a tool like this before claims submission ensures the bill is accurate, the modifiers are justified, and the expected payment aligns with CMS policy.
Poll: Where Do You Usually Get Stuck When Using a Medicare Calculator?
Common Errors When Using Calculators
Even with a powerful tool, it’s easy to make mistakes that skew reimbursement estimates. These errors often lead to underbilling, claim delays, or worse—CMS audits. Avoid these common calculator mistakes:
1. Using Outdated CPT or HCPCS Codes
Each year, Medicare updates the Physician Fee Schedule and code sets. If your code has been deleted or revised, the calculator may return an error—or worse, an inaccurate estimate.
2. Incorrect Modifiers
Missing or misapplied modifiers like -25, -59, or -26 distort how a procedure is reimbursed. Overusing -59, for instance, may trigger compliance red flags and cause bundling issues.
3. Ignoring GPCI
Failing to enter the correct ZIP code or locality will bypass regional adjustments. A $100 procedure in rural Iowa may pay significantly less than the same code in Los Angeles.
4. Confusing Non-Par and Participating Rates
Some calculators estimate limiting charges for non-participating providers. If your practice accepts Medicare assignment, only the allowable amount should be used. Misunderstanding this leads to incorrect billing and patient balance errors.
5. Relying on Default Settings
Always confirm modifiers, POS, and code accuracy. Rushing through entry or using defaults may create false confidence in the estimate. Even a strong calculator won’t correct coding issues at the claim level.
Understanding coding compliance ensures that calculator use aligns with CMS standards and audit expectations. Teams should treat reimbursement estimators as compliance-driven tools, not just convenience features.
| Common Error | Why It Matters |
|---|---|
| Using Outdated CPT/HCPCS Codes | Leads to invalid or inaccurate estimates due to changes in the Medicare Fee Schedule. |
| Incorrect Modifiers | Wrong or missing modifiers like -25 or -59 may trigger bundling issues or claim rejections. |
| Ignoring GPCI/ZIP Code | Excludes regional adjustments, resulting in misaligned reimbursement values. |
| Confusing Participating vs. Non-Par | Applying the wrong rate type can cause billing errors and noncompliance with CMS policies. |
| Relying on Default Settings | Skipping manual input of key fields results in flawed estimates and delayed payments. |
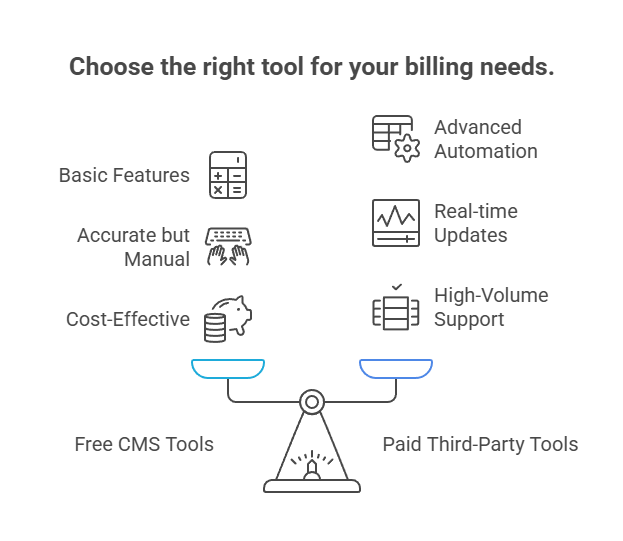
Free vs Paid Medicare Reimbursement Calculators
Not all Medicare reimbursement calculators offer the same depth. While free CMS-provided tools are helpful, third-party platforms often include additional features, automation, and batch capabilities that streamline complex workflows.
Free Tools
CMS offers the Physician Fee Schedule Look-Up Tool, which provides official allowable rates based on CPT/HCPCS codes, modifier use, and geographic locality. It's accurate and authoritative, but not always user-friendly. Users must manually input each data point, and there’s no batch processing or real-time alerts for outdated codes or modifier conflicts.
Free calculators are best suited for single-code lookups, training, or occasional claims checks, especially for small practices or solo billers.
Paid Platforms
Third-party calculators like those embedded in billing software or encoder tools offer advanced features:
Real-time coding updates and CPT validation
Automated GPCI selection by ZIP code
Batch reimbursement estimates for multiple codes
Modifier alerts and compliance prompts
User access logs and role-based permissions
These platforms are ideal for high-volume billers, revenue cycle managers, or coders working across multiple specialties. Many tools also integrate with claim scrubbers and EHRs, saving time and improving coding-to-payment accuracy.
Choosing the right calculator depends on your practice volume, staffing model, and need for automation. For those handling hundreds of claims weekly, investing in a premium tool can prevent thousands in rejected claims and delayed reimbursements.
Comparing coding software terminology helps assess whether a tool supports true compliance logic—or just basic math.
How Medicare Reimbursement Aligns With Private Payers
Medicare’s Physician Fee Schedule doesn’t just affect government billing—it sets the benchmark for private insurance reimbursements across the U.S. Many commercial payers use Medicare’s pricing as the foundation for building their own Usual, Customary, and Reasonable (UCR) rates or contracted fee schedules.
For example, a commercial plan may offer 115% of the Medicare allowable for certain procedures. In these cases, knowing the Medicare baseline helps coders forecast private payer payments more accurately—and flag when contracted rates appear below federal benchmarks.
Some payers adopt Medicare edits and bundling logic outright. This includes NCCI rules, modifier limitations, and GPCI-based regional adjustments. So a Medicare-aligned claim is often more likely to pass cleanly through private payers too.
This alignment is especially critical for multi-payer practices, as errors in one billing model often mirror across others. Using calculators to check Medicare values ensures a stable reimbursement floor and protects against underpricing services in payer negotiations.
For coders prepping for certification, understanding this crossover is vital—especially in CPC exam readiness, where Medicare logic is often tested as a coding baseline.
Private Payers Mirror Medicare Benchmarks
- Most private insurers base rates on the Medicare Fee Schedule
- Typical markups range from 110% to 130% of Medicare rates
- NCCI edits and GPCI logic often reused by commercial payers
- Medicare-aligned claims have higher cross-payer approval rates
- Serves as the pricing floor for payer negotiation
- Helps flag underpriced contracted services
- Vital knowledge for CPC certification prep
- Stabilizes multi-payer billing accuracy
Conclusion
In today’s Medicare landscape, accuracy starts before the claim is even submitted. Reimbursement calculators are no longer optional—they’re essential tools for billing teams that want to reduce denials, forecast revenue, and stay audit-ready. As CMS policies evolve, practices need real-time insight into what Medicare will allow, what modifiers matter, and how reimbursement shifts across locations and services.
These calculators help coders move beyond guesswork. By combining CPT logic, GPCI adjustments, and the current conversion factor, they ensure every estimate is data-driven and compliant. Whether used for single visits or batch claims, the right calculator improves speed, clarity, and financial control.
The best-performing billing teams treat reimbursement estimation as a core part of claim preparation and compliance—not a post-submission fix. With growing complexity across payers and increasing audit pressure, tools like these make the difference between stable cash flow and costly rework.
Frequently Asked Questions
-
The allowed amount is the total Medicare-approved charge for a service. It’s the maximum a provider can be reimbursed—regardless of who pays. The paid amount is what Medicare actually pays after subtracting the patient’s share. Typically, Medicare covers 80% of the allowed amount, and the patient is responsible for the remaining 20% (coinsurance) after their deductible is met. For participating providers, billing more than the allowed amount is prohibited. For non-participating providers, a limiting charge cap applies. Accurately estimating both figures helps billing teams forecast payments and avoid patient billing errors.
-
It depends on the platform. Free CMS tools generally allow single-code lookups, requiring manual repetition for each service. However, most paid calculators or EHR-integrated tools support batch entry of multiple CPT or HCPCS codes. These advanced tools calculate totals, flag modifier conflicts, and adjust for bundling or code interdependencies. For high-volume billers, batch calculators significantly speed up claim prep and reduce entry errors. Batch features are especially useful for encounters involving multi-component services, such as surgical bundles, DME packages, or complex outpatient visits.
-
Medicare updates its Physician Fee Schedule (PFS) annually, with new rates typically going into effect every January 1. These updates include changes to conversion factors, RVUs, and covered services, along with coding and modifier revisions. Mid-year updates can also occur for emergency legislation or CMS corrections. Staying current is critical—using outdated CPT codes or values can result in denied claims, inaccurate estimates, or compliance violations. Most professional billing platforms integrate automatic updates. For manual workflows, always download the most recent CMS PFS release before running estimates.
-
Yes—most reputable calculators automatically apply the Geographic Practice Cost Index (GPCI) based on ZIP code or selected locality. This ensures that each CPT or HCPCS code is adjusted according to the regional cost of providing care. GPCI accounts for variations in labor, rent, malpractice insurance, and overhead by region. However, some calculators require users to manually select their locality, while others detect it automatically. Forgetting to apply GPCI will result in inaccurate reimbursement figures, especially for providers billing in high-cost metro areas or underserved rural zones.
-
Calculators themselves don’t guarantee compliance—but they support it when used correctly. By ensuring CPT codes are valid, modifiers are accurate, and RVUs are correctly calculated, these tools help produce clean, audit-ready estimates. Many paid calculators also log user entries, store historical lookups, and flag known CMS bundling or denial triggers. Used as part of a broader compliance workflow—including proper documentation and claim review—they help reduce errors that might otherwise lead to post-payment audits or recoupment demands. However, they must be paired with updated coding guidance, payer rules, and clear internal protocols.