Mastering Specialty Coding Exams: Cardiology & Vascular Coding
Specialty coding certifications are no longer optional — they’re a strategic move for career security and advancement. As payer policies tighten and compliance audits become more aggressive, coders who specialize in high-risk domains like cardiology and vascular care are earning more and getting hired faster. These fields are procedure-heavy, modifier-sensitive, and require coders who can interpret nuanced clinical scenarios with near-clinical precision.
Cardiology and vascular coding roles often report higher average salaries than generalist coders because of the demand for accurate interpretation of complex CPT groupings, bundled payment logic, and ICD-10 specificity in chronic conditions. Hospitals, payers, and RCM firms are prioritizing certified coders who can handle cardiac catheterizations, stent placements, electrophysiology, and vascular anomalies without triggering denials. As a result, mastering these specialties doesn't just future-proof your career — it positions you at the top tier of medical coding roles.
Understanding Cardiology Coding Frameworks
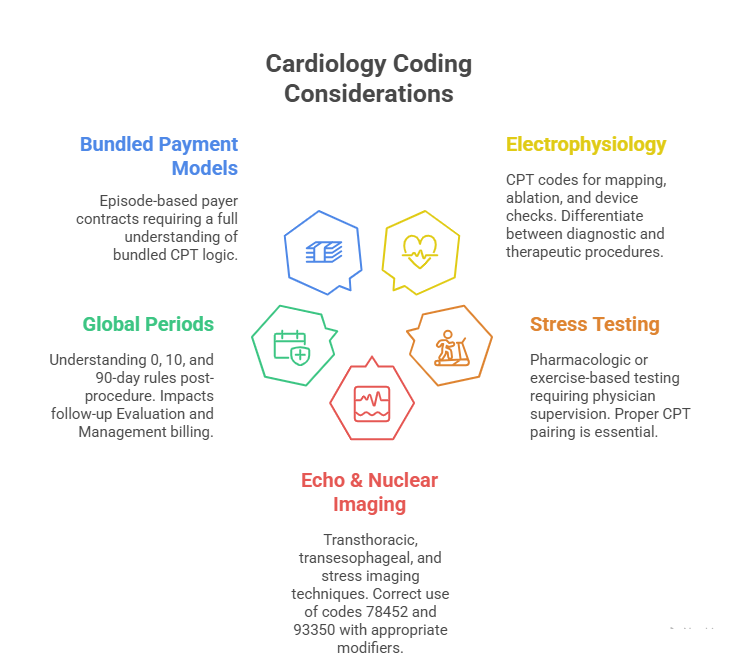
Cardiology coding requires a framework that aligns with both clinical intent and payer logic. Unlike general E/M coding, cardiology involves interpreting high-complexity procedures that span diagnostic, interventional, and post-procedural stages. This makes precision essential. Coders must navigate layered documentation, overlapping services, and distinct global periods without missing a modifier or CPT pairing.
The specialty is CPT-dense and highly scrutinized, especially when it comes to electrophysiology, catheterizations, stent placements, and imaging-guided procedures. Each segment within cardiology has its own coding rhythm — and failing to follow it leads to denials, audit flags, and compliance risk. Below is a deeper look into the core areas:
CPT Codes in Electrophysiology, Stress Tests, etc.
Electrophysiology coding involves a matrix of codes that reflect mapping, ablations, device checks, and lead implantations. Coders must differentiate between diagnostic EP studies (e.g., 93620, 93621) and therapeutic interventions (e.g., 93653 for ablation). Many denials happen when documentation doesn't reflect inducible arrhythmia or fails to support the level of mapping performed.
Stress test coding also requires attention to specificity — whether pharmacologic (93015–93018) or treadmill-based, and who supervises the test (physician vs technician). CPT descriptors are granular. For example, a nuclear stress test may require combining codes like 78452 (nuclear imaging) and 93017 (physiologic monitoring) for proper reimbursement. Each component must be reported correctly with proper modifiers, especially when done in split-location settings (e.g., physician office vs hospital outpatient).
Global Periods and Bundled Payments
One of the biggest coding challenges in cardiology is understanding which services are included in the global surgical package and which aren’t. Interventional cardiology procedures often come with 90-day global periods, meaning follow-up visits, rechecks, and certain diagnostics are bundled unless specifically excluded.
Coders must distinguish between pre-op, intra-op, and post-op services. For example, evaluation before a cardiac cath (CPT 93458) is bundled unless it's unrelated to the planned intervention. Billing for a 99214 during a global period without modifier -24 can trigger an automatic denial or audit.
Bundled payments also apply to cardiology episodes in many payer contracts. Understanding episode-of-care logic, including care coordination codes (99487–99489) or transition codes (99495–99496), can help capture revenue often missed under standard fee-for-service logic.
Coders who master these frameworks elevate their value — not just by preventing losses, but by unlocking billable services that others miss. That's what sets apart top-performing cardiology coders from generalists.
Vascular Coding Essentials and Pitfalls
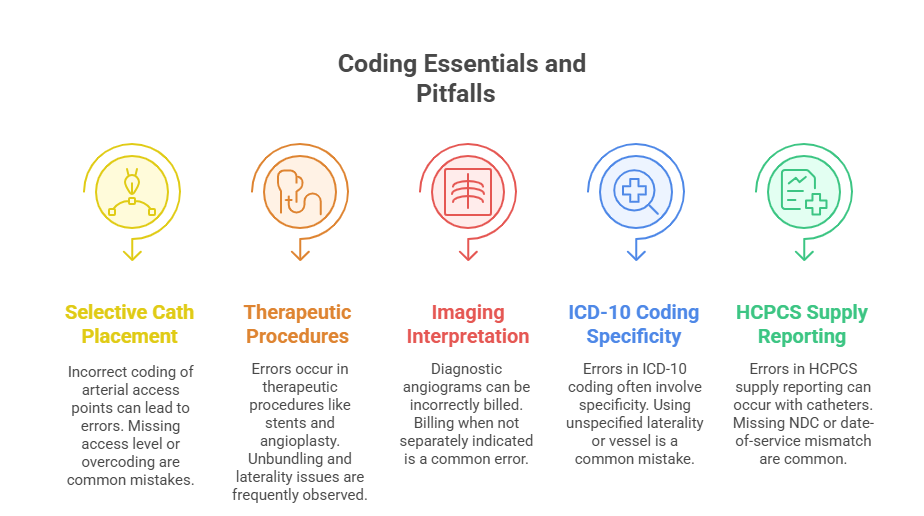
Vascular coding is one of the most error-prone specialties due to overlapping procedures, multiple anatomical sites, and strict payer rules. Coders must be fluent in distinguishing between diagnostic imaging and interventional treatments, especially when both occur in the same session. The CPT guidelines for vascular procedures are highly scenario-specific, and missteps here often lead to undercoding or denial triggers.
Unlike general outpatient coding, vascular services deal with complex hierarchies of selective catheter placements, arterial access routes, and multiple territory rules. Coding accurately in this space means being able to read operative reports line-by-line — knowing when to apply codes like 37226 (femoral stent) versus 36247 (selective cath placement), and when to avoid unbundling procedures already captured within global descriptors.
Common Denials and Billing Mistakes
The most frequent vascular denials occur due to:
Unbundling errors: Attempting to bill separately for procedures already included in a comprehensive CPT code.
Missing laterality/modifier details: CPT and ICD-10 codes often require specificity about left/right sides and anatomic location (e.g., iliac vs femoral).
Unsupported imaging codes: Reporting 75710 (angiography) without proper documentation showing necessity and interpretation.
Improper sequence coding: Failing to prioritize catheter placement codes before therapeutic interventions.
Payers often cross-check CPTs against procedure-to-modifier logic. Submitting 59 modifiers for related procedures without documentation justification almost always gets flagged. Some MACs even reject claims when modifiers aren’t placed in the correct order, regardless of medical necessity.
Another pitfall: coders misinterpret terminology like "angioplasty" or "revascularization," applying broad stroke codes that miss technical specificity. For example, transluminal balloon angioplasty requires different CPT logic than atherectomy or thrombectomy — and the site hierarchy matters in every single case.
ICD-10/HCPCS Applications in Vascular Settings
Vascular coding demands ICD-10 fluency in chronic conditions like PVD (Peripheral Vascular Disease), atherosclerosis, and post-operative sequelae. Coders must map diagnoses to procedures with precision. A common error is assigning I70.219 (atherosclerosis of native arteries) generically when specificity exists — such as I70.233 (right leg with ulceration).
HCPCS codes also play a major role in vascular settings — especially for stents, catheters, contrast agents, and compression therapy supplies. These are often billed separately under outpatient billing (e.g., hospitals or ASCs) and impact total claim reimbursement. Coding professionals must align HCPCS supply coding with the date of service, NDC compliance, and modality used.
Those who master this complexity become essential to vascular teams. Their coding prevents downstream denials, recovers missed revenue, and protects practices from compliance risk.
Required Knowledge for Specialty Exams
Specialty coding exams in cardiology and vascular domains are designed to test for technical precision, regulatory awareness, and scenario-based CPT judgment. These aren't entry-level assessments — they require coders to think like both clinicians and auditors. Whether you're sitting for AAPC's CCC (Certified Cardiology Coder) or preparing through AHIMA-aligned courses, the emphasis is on how well you handle complexity under pressure.
Exams simulate real-world claim reviews. Expect to be tested on bundled service logic, selective catheter placements, high-risk modifiers, and compliance protocols like NCCI edits, MUE limits, and payer-specific rules. Time pressure is intense, and many fail not due to lack of knowledge, but due to misjudging documentation cues or missing sequence rules.
What AAPC and AHIMA Exams Test For
The AAPC Certified Cardiology Coder (CCC) exam focuses heavily on CPT accuracy, especially in:
Interventional cardiology: stents, caths, angioplasties
Electrophysiology: ablations, pacers, defibrillators
Stress tests and echocardiography: including Doppler and transesophageal studies
Candidates must demonstrate deep understanding of modifier use, global periods, and when to break bundling rules. Case scenarios often involve documentation that’s intentionally ambiguous — your job is to extract correct codes, even if details are implied rather than explicitly stated.
AHIMA's approach emphasizes clinical documentation integrity (CDI), ICD-10 mastery, and audit-readiness. If you’re pursuing vascular specialties through AHIMA, expect a heavier focus on diagnosis-to-procedure matching, HCPCS supply codes, and payer denial management strategies.
Both exams test your ability to apply payer policies, not just coding guidelines. That includes knowing when a modifier triggers a bypass edit, or when an NCCI pair is only allowed in different anatomic sites.
Recommended Prep Materials
Top resources for cardiology and vascular exam prep include:
AAPC’s CCC Study Guide: Tailored for interventional and diagnostic cardiovascular coding. Includes bundled coding maps and test-format scenarios.
CPT® Professional Edition (Current Year): Vital for understanding parenthetical instructions, global notes, and procedural crosswalks.
ICD-10-CM Expert: Use a version that includes guideline callouts and chronic condition coding notes.
HCPCS Level II Expert Manual: Especially for outpatient and supply coding references.
Practice exams and case scenario workbooks: Ideally ones that include documentation snippets and CPT/ICD interlinking logic.
Coders preparing without hands-on practice are at a disadvantage. Successful candidates spend 20–40 hours on case-based drills, modifier trees, and denial root-cause matching — not just flashcard memorization.
| Area | What to Know | Tested By |
|---|---|---|
| Cardiac Caths & EP Studies | Full procedural coding, modifier logic | AAPC CCC exam |
| Global Period Applications | CPT timing rules and included services | AAPC & AHIMA |
| ICD-10 Mapping | Chronic condition linkage and risk flagging | AHIMA exams |
| HCPCS & Supplies | Matching procedures with materials billed | CPB exam crossover |
| Documentation Evaluation | Identifying billable elements in ambiguous notes | Both AAPC and AHIMA |
Real-World Application in Practice Settings
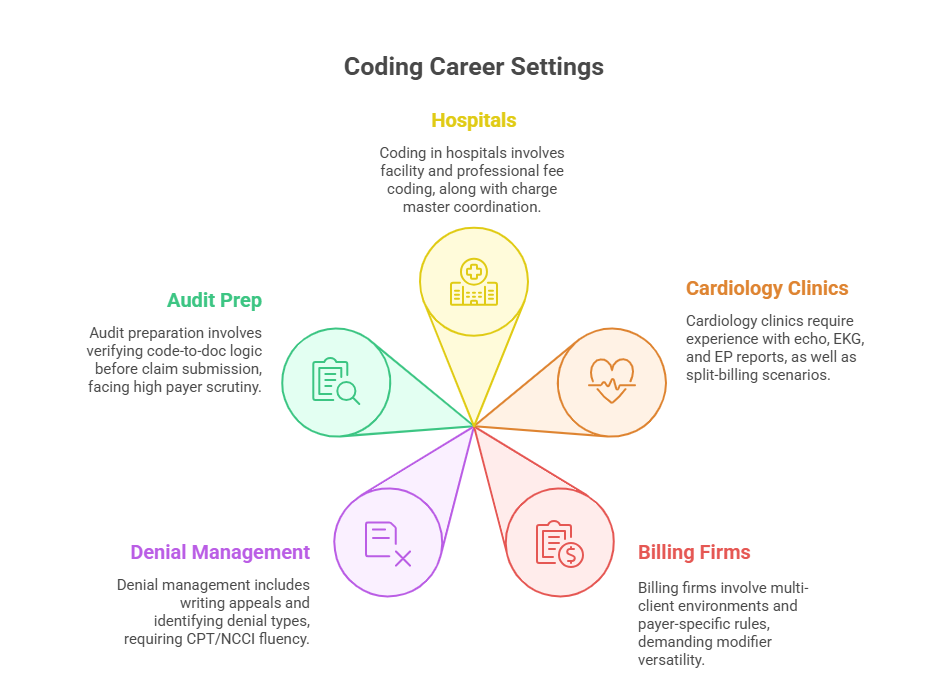
Specialty coding knowledge is only as valuable as its real-world application. In cardiology and vascular settings, coders are the gatekeepers of revenue integrity, claim survivability, and audit resilience. The documentation is often verbose, but the billable elements are buried in brief notes, imaging interpretations, or catheter lab reports. This requires coders to extract not just data — but reimbursable precision.
Whether you’re working with hospitals, clinics, or billing firms, the environment is fast-paced, compliance-driven, and revenue-sensitive. Coders are expected to flag errors pre-claim, communicate with providers for addenda, and ensure coding aligns with payer policies and LCD/NCD rules. In vascular work, even the anatomy terminology used in the procedure note can make or break payment.
Hospitals, Cardiology Clinics, Billing Firms
In hospitals, especially in the cath lab or EP units, coders must navigate hybrid models — a mix of inpatient ICD-10-PCS for facility billing and CPT for professional billing. You’ll often coordinate with charge masters, revenue cycle teams, and clinical documentation specialists. The workload is higher, but so are the expectations.
In cardiology clinics, coders often work side-by-side with physicians. You’ll review procedural notes, attach modifiers like -26, -59, or -XS, and ensure services like echo-guided interventions or ambulatory rhythm monitoring are fully captured. Denials here are most common for lack of supporting diagnosis or inappropriate sequencing.
For remote billing firms or third-party RCM providers, coders need multi-client adaptability. You’ll encounter different EMRs, varied payer contracts, and documentation styles ranging from robust to chaotic. The skill here lies in applying universal logic with client-specific nuance, especially when dealing with bundled contracts and risk-adjusted models.
Managing Denials and Insurance Reviews
Even expert-level coding can’t avoid every denial — which makes proactive denial management a vital skill. Most cardiovascular denials occur due to:
Missing or misused modifiers
Undocumented medical necessity
Unclear or inconsistent provider documentation
Global period rule violations
Coders must know how to write appeals that reference CPT Assistant, payer policy, and NCCI edits directly. Appeals should never rely on emotion — they must rely on technical specificity. You’re not just coding; you’re building an evidence-backed defense.
Insurance reviews may request operative reports, progress notes, and imaging reads. Coders who can quickly extract those details and present code-level justification often determine whether the claim gets paid or rejected. Mastery of these workflows is what turns coding into a career asset, not just a task.
Salary Trends for Specialty Coders
Specialty medical coders consistently earn 15–30% more than generalist coders, and those certified in cardiology or vascular coding often land in the top salary brackets of the profession. The rise in value stems from two key drivers: increasing complexity in cardiovascular care and stricter payer scrutiny. Coders who understand high-risk specialties are no longer viewed as backend staff — they’re frontline revenue defenders.
Pay rates are especially favorable for those who combine specialty knowledge with national certifications, such as the CPC or CPB. In fact, certified coders with cardiovascular specialization can command $65,000–$90,000/year depending on location, experience, and work setting — compared to the $50,000–$60,000/year average for general coders.
Comparison With General Coders
General medical coders often work in family practices, urgent care, or general outpatient services. Their work leans heavily on E/M leveling, preventive care documentation, and ICD coding for common conditions. While foundational, these areas don’t carry the same weight in terms of complexity or compliance risk.
Specialty coders, by contrast, manage:
Multi-component procedures (e.g., cath with stent and imaging)
High-frequency modifier logic (e.g., 59, XS, XU, 91)
Technical procedural groupings with strict bundling rules
Because errors in these domains result in higher dollar losses, employers are willing to pay a premium for accuracy. RCM firms, hospitals, and cardiology clinics often prioritize coders with niche expertise during hiring, even over those with longer generalist experience.
Location and Certification-Based Variances
Salary potential also fluctuates based on geographic region and certification level. In major metro areas (e.g., New York, Los Angeles, Houston), specialty coders often break $90,000/year with less than 5 years of experience — especially when working with hospital systems or academic centers.
In contrast, rural coders may see slightly lower salaries but enjoy remote flexibility, contract work, or travel opportunities through firms needing nationwide expertise. Credentialed coders with dual certifications — especially those who’ve completed programs like the AMBCI Dual CPC + CPB Certification — tend to rank higher on salary ladders due to their ability to code, audit, and bill across multiple domains.
As payer models evolve into value-based care and risk-adjusted reimbursement, specialty coding will no longer be optional — it will be a minimum threshold for earning at the top of the profession.
| Factor | Impact on Salary | Data Point |
|---|---|---|
| Specialization (Cardiology) | Increases salary by 15–30% | Higher claim complexity |
| Certification Level | Dual CPC + CPB or CCC boosts earnings potential | $70K+ averages |
| Location | Metro coders earn more; rural coders gain flexibility | NYC vs Midwest gap |
| Experience | 3+ years in specialty yields fast pay progression | Rapid seniority in niche roles |
| Work Setting | Hospitals and academic centers pay more than private clinics | Institutional budget differences |
How AMBCI’s Dual CPC + CPB Course Prepares You
The AMBCI Medical Billing and Coding Certification is engineered for professionals aiming to master specialty domains like cardiology and vascular coding while building foundational strength in both CPT and insurance billing workflows. Unlike generic CPC prep programs, this dual certification goes deeper — offering 200+ specialty modules, including case-based lessons that mirror real-world cardiology encounters.
You won’t just memorize codes — you’ll learn how to interpret operative reports, apply global period logic, navigate ICD-10 for chronic cardiac conditions, and manage HCPCS Level II supply coding for vascular devices. Each lesson integrates AAPC exam prep, complete with scenario-based drills on electrophysiology, cardiac caths, and bundled service breakdowns. This mirrors exactly what’s tested in real CPC and CPB exams.
What truly sets AMBCI apart is its billing integration. You’re not just learning to code — you're being trained to analyze denials, build clean claims, and justify modifier decisions with payer language. That’s what employers are looking for when hiring for cardiology departments, RCM firms, or hospital billing teams.
If you're serious about specialty coding — and want to be seen as certification-ready and employer-preferred — the AMBCI dual certification gives you the toolkit, the credential, and the specialty focus to stand out.
Frequently Asked Questions
-
General coding focuses on evaluation and management (E/M), common diagnoses, and procedural codes used in routine healthcare settings. Cardiology coding, on the other hand, involves highly specific CPT codes for electrophysiology studies, stent placements, cardiac catheterizations, and bundled services with defined global periods. It requires a deep understanding of modifier logic, anatomical specificity, and payer rules unique to cardiovascular care. Coders must interpret complex reports, identify billable procedures from layered notes, and apply nuanced guidelines that generalists are often not trained in. As a result, cardiology coding offers higher salaries, more job stability, and is increasingly sought after in specialized healthcare environments.
-
Cardiology and vascular coding involve interpreting high-risk procedures with strict payer oversight and layered documentation. These services are typically modifier-heavy, bundling-sensitive, and carry higher claim values, which increases financial risk for providers. Employers pay more for coders who can prevent denials and ensure compliance in these critical specialties. Additionally, certified coders in these areas often handle both coding and appeals, further boosting their role in revenue cycle management. Specialty certifications signal a higher level of competence, making candidates more competitive and better compensated across hospitals, cardiology clinics, and RCM firms.
-
The most common mistakes include unbundling services already included in comprehensive CPT codes, misplacing modifiers, and coding without proper anatomical specificity. Many denials arise from incorrect use of codes like 37220–37235, where the distinction between stent, angioplasty, and atherectomy isn’t documented clearly. Other frequent issues include missing laterality indicators in ICD-10 codes (e.g., right vs. left leg) and improperly billing for diagnostic angiograms when they’re not separate from the primary procedure. Documentation mismatch between the operative note and the submitted codes also triggers payer rejections or audits. Mastery in this area demands both technical skill and anatomical accuracy.
-
To prepare effectively for the AAPC CCC exam, focus on case-based CPT scenarios, especially in areas like cardiac catheterizations, ablations, and pacemaker placements. Practice identifying when diagnostic services are bundled versus separately billable. Use the AAPC CCC Study Guide, current CPT and ICD-10 manuals, and scenario workbooks with real-world documentation excerpts. Prioritize understanding global periods, modifier -59 use, and when to override NCCI edits. Weekly mock exams under timed conditions can build speed and accuracy. Also review denial scenarios and appeals writing, since understanding claim survivability logic is crucial for exam success and real-world application.
-
Yes, but only with rigorous training. While you don’t need to be a clinician, vascular coding requires understanding of vascular anatomy, procedure intent, and how catheter placements relate to intervention codes. High-quality training programs like the AMBCI Medical Billing and Coding Certification offer modules that break down complex operative notes into digestible codeable components. Visual anatomy guides, case study reviews, and modifier application drills bridge the gap between clinical action and coding logic. Without structured training, self-teaching vascular coding can lead to dangerous overcoding or revenue loss, especially in high-dollar, high-denial settings like interventional radiology or endovascular labs.
-
Top cardiology CPT codes include:
93458 – Cardiac catheterization with coronary angiography
93653 – Electrophysiologic study with ablation
93015–93018 – Stress test codes (supervision, tracing, and interpretation)
33208 – Pacemaker insertion, dual chamber
78452 – Myocardial perfusion imaging (nuclear stress test)
Each of these requires careful review of the clinical scenario, documentation, and setting. Modifier use (e.g., -26, -59) and global period considerations apply. Coders must verify which components are bundled and whether supervision or technical components can be billed separately. Misuse of these high-value codes is one of the top triggers for payer audits and revenue leakage in cardiovascular settings.
-
Yes. The AMBCI Medical Billing and Coding Certification includes over 200 specialty modules, with in-depth lessons on cardiology and vascular coding. These modules simulate real-world scenarios involving catheter placements, stress testing, pacemaker insertions, and angioplasty/stenting procedures, giving learners hands-on exposure before entering the workforce. Lessons integrate AAPC exam prep, case-based CPT walkthroughs, and denial resolution workflows. It also includes billing simulations that show how coding decisions affect claim outcomes, reimbursement, and compliance flags. This makes AMBCI’s program ideal for coders who want immediate job readiness and credentialed proof of specialization.
-
Effective denial management begins with accurate pre-claim coding and awareness of payer-specific bundling policies. When denials occur, coders should first confirm whether the issue was documentation-related, modifier-based, or payer policy-driven. For example, missing modifier -25 on an E/M during a global period is a common trigger. Strong appeals reference CPT Assistant, NCCI edits, and payer LCD/NCD guidelines, not just a restatement of facts. Coders should maintain a denial log, categorize denial types, and build templates for appeal letters tailored to each payer. This proactive approach ensures faster resolution, fewer repeat issues, and improved practice cash flow.
The Takeaway
Cardiology and vascular coding aren’t just advanced specialties — they’re career accelerators. As payer scrutiny intensifies and procedure complexity rises, certified specialists are becoming indispensable assets to hospitals, clinics, and billing firms. These domains demand more than surface-level coding; they require clinical insight, technical mastery, and claim-level precision.
Mastering these niche areas doesn't just increase your value — it protects your career from automation, positions you for remote and leadership roles, and connects you to higher-paying job markets. With the right preparation, especially through programs like the AMBCI Medical Billing and Coding Certification, coders can move from reactive claim handling to proactive revenue leadership. In a profession where accuracy equals income, specialty coding is where growth happens — and where coders thrive.