How to Become an Oncology Coding Specialist
Oncology coding is where tiny documentation choices move six-figure revenue—and where auditors live. If you want employers and practices to trust you with chemo regimens, radiation plans, and complex bundling, you need outcome-driven skills, flawless compliance habits, and a roadmap that turns months of study into billable competence. Use this guide to map credentials, master tumor-site specifics, standardize SOPs, and publish measurable wins. Cross-link your learning with AMBCI pillars such as coding compliance trends, future skills in the age of AI, and ICD-11 infectious disease guidance to outpace market change fast.
1) Why oncology coding is different—and how to show value in 30–60 days
Oncology coding touches chemotherapy administration, immunotherapy, radiation therapy, surgery, and palliative/infusion services—often in the same episode. Denial drivers include wrong drug units (J-codes), compound wastage documentation, imprecise laterality/staging, and global period conflicts between med-onc, rad-onc, and surgery. Your first objective is to lower denial volume and raise first-pass clean claims quickly.
Immediate “win zones” to demonstrate value:
Drug unit accuracy and wastage documentation. Build a crosswalk that maps HCPCS drug codes to common vial sizes and wastage rules; pair with payer-specific policies. Publish a one-pager and link it to predictive analytics opportunities so leaders see how you’ll flag outliers before submission.
Staging + tumor site precision. Maintain ICD-10-CM libraries with site/laterality granularity and oncology staging indicators; tie this to medical necessity narratives reinforced by CMS compliance fundamentals.
Modifier integrity. Codify when to use 59/XS, JW, and RT/LT; minimize NCCI conflicts through prebills aligned with compliance trend monitoring.
Site-specific “fast packs.” Build tumor-type cheat sheets (breast, lung, colorectal, prostate, hematologic) and map them to career acceleration via CE.
Show value fast by running a 30-day denial rescue: audit 100 recent denials, classify CARC/RARC patterns, write payer-specific fix SOPs, and present overturned revenue in a QBR. Reference AMBCI playbooks on automation’s impact on billing roles and remote job trends to position yourself as the coder who reduces risk while scaling capacity.
| Focus Area | Typical Codes/Concepts | What to Standardize | Common Denials | Fast KPI to Track | Helpful Add-On |
|---|---|---|---|---|---|
| Chemo admin—initial | 96413 | Time thresholds; route | CO-97, MUE | +1st-pass rate | Infusion log template |
| Chemo admin—addl hr | 96415 | Infusion documentation | Units mismatch | –RARC N59 | Timer checklist |
| Chemo push | 96411/96409 | Push vs infuse rules | NCCI edits | –edit hits | Route crosswalk |
| Therapeutic infusion | 96365–96368 | Hierarchy selection | Upcoding | Audit pass % | Hierarchy flowchart |
| Hydration | 96360–96361 | Clinical necessity | Bundling | –CO-50 | Clinical criteria sheet |
| Immunotherapy | J9271+ (e.g., pembrolizumab) | Drug units; wastage | JW misuse | 0 JW errors | Vial/units map |
| Anti-emetics | J2405, J1453 | Supportive therapy rules | Med nec | –CO-50 | Order set link |
| Growth factors | J2506 (pegfilgrastim) | Same-day modifiers | POS errors | 0 POS denials | POS crosswalk |
| Oral oncolytics | S codes, NOC billing | Coverage by payer | Plan exclusion | Appeal success | Appeal letter kit |
| Chemo wastage | JW modifier | Wastage note format | Missing wastage | 0 JW recoup | Wastage template |
| Port access | 36591/36592 | When separately payable | Bundling | Correct usage % | Decision tree |
| Biopsy—breast | 19081–19086 | Imaging guidance | Laterality | 0 laterality denials | Laterality checklist |
| Onc surgery bundling | Modifier 58/78/79 | Global rules | Global conflicts | –global edits | Global period table |
| Radiation planning | 77261–77263 | Plan complexity | MUE | Plan code accuracy | Plan doc template |
| Radiation delivery | 77402–77412; 77427 | Fractions tally | Units mismatch | 0 unit errors | Fractions tracker |
| SRS/SBRT | 77371–77373; 77372 | Episode bundling | Incorrect combo | Audit pass % | SRS checklist |
| Hematology workups | 85025; 88184–88189 | Panel rules | Overlapping panels | –duplicate billing | Panel map |
| Pathology margins | 88307–88309 | Specimen vs block | Units confusion | Block/unit accuracy | Specimen log |
| Genetic testing | 81211–81217 (BRCA) | Coverage criteria | Non-covered | Auth success | Auth script |
| Staging indicators | ICD-10 Z85/Z86; Cxx | Primary vs secondary | History vs active | 0 Z-code misuse | Staging grid |
| Telehealth oncology | POS 02/10; 95/GT | POS accuracy | POS denials | 0 telehealth denials | POS crosswalk |
| Palliative care | 99497–99498 | Time & consent | Time deficit | Time doc accuracy | Time tracker |
| ERAS/chemo teach | 98960–98962 | Education qualifiers | Med nec | Paid education % | Qualifying note |
| Clinical trials | Q0/Q1; modifier 59 | Trial IDs & modifiers | Missing trial data | 0 trial denials | Trial field set |
| Sepsis w/ malignancy | A41.x + Cxx; R65.2x | Principal selection | POA/status errors | DRG accuracy | Principal picker |
| Anemia due to chemo | D64.81 + T45.1X5A | Adverse effect chains | Linkage gaps | Linkage correctness | Linkage cheat sheet |
| Malnutrition w/ cancer | E43–E46 | Severity capture | Downcoding | CC/MCC capture | RD note prompts |
2) Credentialing & study roadmap: from CPC/CCS to oncology-ready
Start with a core credential—CPC or CCS—to signal baseline competence. From there, build an oncology pathway with three tracks run in parallel:
Track A — Documentation outcomes. Use E/M refreshers, chemo admin hierarchies, and claim-edit knowledge to create measurable wins. Reinforce with continuing education accelerators and test efficiency with practice test methods.
Track B — Compliance mastery. Internalize payer and CMS expectations, medical necessity, and NCCI. Follow compliance trends, then build a personal audit log that would satisfy any payer. Pair this with HIPAA SOPs and remote-work guardrails influenced by remote career guides.
Track C — Tumor-site depth. Each quarter, pick two tumor types (e.g., breast and lung). Build decision trees for code selection, laterality, staging, and surgery bundling; connect to modifier optimization and craft payer-specific appeal packets.
If you’re transitioning from general coding or aiming at leadership, cross-plan with HIM pathways and revenue cycle management roles. For long-term relevance, keep a quarterly theme around AI in RCM so you can evaluate tooling rather than be replaced by it.
3) Build site-specific mastery: breast, lung, colorectal, prostate, hematologic
Breast cancer. Focus on biopsy codes (19081–19086) with imaging guidance, margin assessments (88307+), and laterality. Tie surgical sequences to global period rules and modifiers 58/78/79. Use payer bulletins to differentiate mastectomy subtypes and reconstruction coding. Publish a micro-guide and interlink with compliance resources and emerging job roles.
Lung cancer. Pre-op staging with bronchoscopy (31622–31628) and EBUS (31652–31653) demands precise add-on usage. Distinguish primary vs secondary malignancies and document tobacco dependence. For rad-onc, map fractions and capture 77427 correctly. Cross-link with predictive analytics for outlier detection.
Colorectal. Colonoscopy polypectomy methods (snare vs hot biopsy) profoundly change coding; maintain a method map. In hospitalization, code complications (e.g., postoperative ileus) with status indicators. Tie to nutrition status (E43–E46) for CC/MCC capture, then reference ICD-11 infectious disease guidance when immunosuppression interacts with infections.
Prostate. Understand androgen-deprivation drug rules, imaging (PSMA PET), and radiation regimens. Build a grid of drug units/vial sizes and link to modifier JW logic. Validate POS for telehealth consults using remote work frameworks.
Hematologic malignancies. Track complex lab panels (flow cytometry 88184–88189), transfusions, and bone marrow procedures. Build “adverse effect” chains for chemo-induced anemia (D64.81 + T45.1X5A) and neutropenia (D70.1), then align education with career-accelerating CE.
Wrap these packs into a weekly learning cadence. Each “pack” should include: code map, denial patterns, appeal language, and provider prompts, then be benchmarked against KPIs from the table above.
Quick Poll: Which oncology pain point blocks clean claims most?
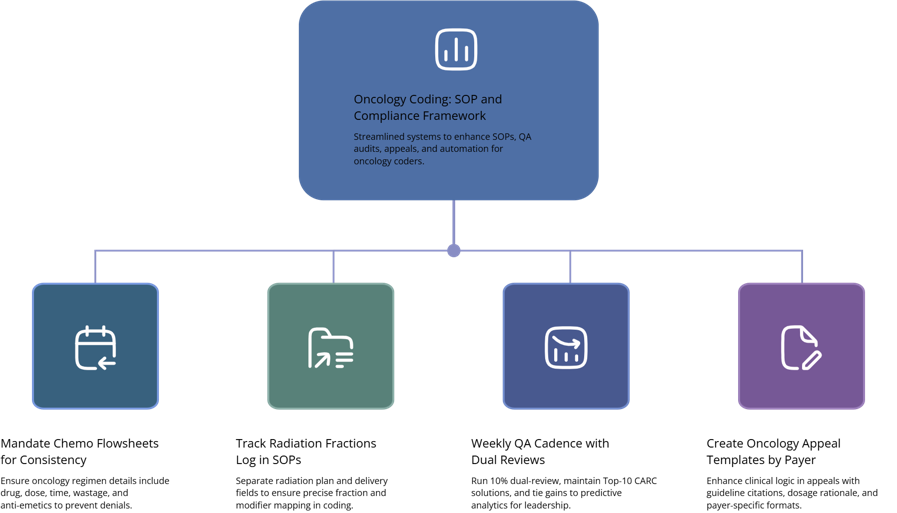
4) SOPs, QA, and compliance: the oncology coder’s operating system
Standardize inputs. Oncology denials often start with missing regimen details, fractional mismatches, or vague staging. Mandate a chemo flowsheet with drug, dose, units, start/stop times, wastage, and anti-emetics. For radiation, enforce a fractions tracker and plan/delivery separation. Map every intake field to a code or modifier choice. Tie your SOPs to AMBCI’s compliance frameworks and embed change monitoring using upcoming regulatory change posts.
QA cadence. Run a 10% dual-review every week and maintain a rolling “Top-10 CARC” playbook. For each CARC, keep: definition, trigger pattern, payer quirks, fix steps, and appeal language. Connect measured gains to predictive analytics so leadership can see future risk reduction.
Appeals excellence. Oncology appeals succeed when clinical logic is explicit. Build templates that include regimen rationale, guideline citations, and drug unit math. Maintain versions by payer and align with modifier optimization guidance.
Trial coding controls. Require trial IDs in a dedicated field; enforce Q0/Q1 modifiers and diagnosis sequencing. Keep a monthly audit specifically for trials. Document decisions and distribute a two-page brief as part of your compliance program linked to coding compliance trends.
Telehealth realities. Oncology adds many virtual touchpoints (treatment plan discussions, toxicity checks). Enforce POS 02/10 rules and 95/GT as required. Validate visit types and counseling time. Leverage remote coding trend guidance to keep POS errors at zero.
Human + automation. Use tech for units math, NCCI prechecks, and fraction counts; keep edge cases human. Position yourself using AMBCI’s AI/automation outlook so stakeholders trust your oversight rather than fear replacement.
5) Career pathways, compensation, and advancement (clinic, hospital, payer)
Entry path (0–1 year oncology). With CPC/CCS and targeted oncology packs (chemo, breast, lung), apply for oncology coder or infusion coder roles. To stand out, showcase a 60-day plan and link it to AMBCI guides like career roadmaps for coders and state salary benchmarks. If you’re in competitive markets (CA/FL), tailor outreach with California job insights and Florida outlooks.
Mid-career (2–4 years). Shift into denials analytics lead or oncology QA specialist and own the CARC playbook. Translate wins (–25–35% denials, 0 JW recoups) into published case studies. Keep advancing via continuing education and site-specific expertise.
Senior/lead (5+ years). Options include oncology coding educator, clinical trials documentation specialist, rad-onc coding lead, or broader RCM leadership. If you want management, align your skill story with revenue cycle manager guides or transition toward HIM leadership paths. Hedge against disruption with AI-aware process design grounded in RCM automation trends.
Freelance/consulting track. Oncology niches monetize well in freelance form. Start with a chemo unit integrity audit or radiation fraction compliance sprint, price against KPIs, and retain with monthly QA. Benchmark price with AMBCI salary pages and position your services as remote-friendly using globalization of coding jobs insights.
6) FAQs — oncology coding, clarified
-
Start with CPC or CCS to signal general competence, then stack oncology-specific mastery (chemo admin, drug units, radiation). Reinforce your credibility through continuing education and a public CARC playbook grounded in compliance trends. Publish 2–3 short case studies with measurable denial reduction.
-
Standardize units math, wastage notes (JW), and anti-emetic rules; align drug units to vial sizes and maintain a payer-specific matrix. Run NCCI prechecks, and design intake templates mapping each field to billing logic. Validate your approach with predictive analytics guidance and modifier optimization.
-
Split your plan into planning (77261–77263), simulation, dosimetry, and delivery (77402–77412, 77427). Build a fractions tracker and a unit audit. Review payer MUEs monthly. Tie your updates to regulatory change monitoring and maintain a QBR slide showing error trends.
-
Require trial IDs, apply Q0/Q1 properly, and ensure correct sequencing of diagnoses and modifiers. Keep dedicated appeal language. Publish your trial SOP and link it to compliance guidance so auditors see a consistent standard.
-
Automation catches unit math and edit patterns, but humans write medical-necessity narratives, resolve edge cases, and craft successful appeals. Upskill along AMBCI’s future-skills roadmap and apply AI/RCM trend insights to design human-in-the-loop QA that buyers trust.
-
List first-pass rate, denials per 100 claims, JW error rate (target = 0), appeal overturn %, radiation unit accuracy, and trial compliance score. Reference AMBCI’s state salary guide to contextualize your value story by geography.